Imagine your newborn was constantly in pain, so much so that they barely slept. This was our family’s reality for the first year of our daughter’s life.
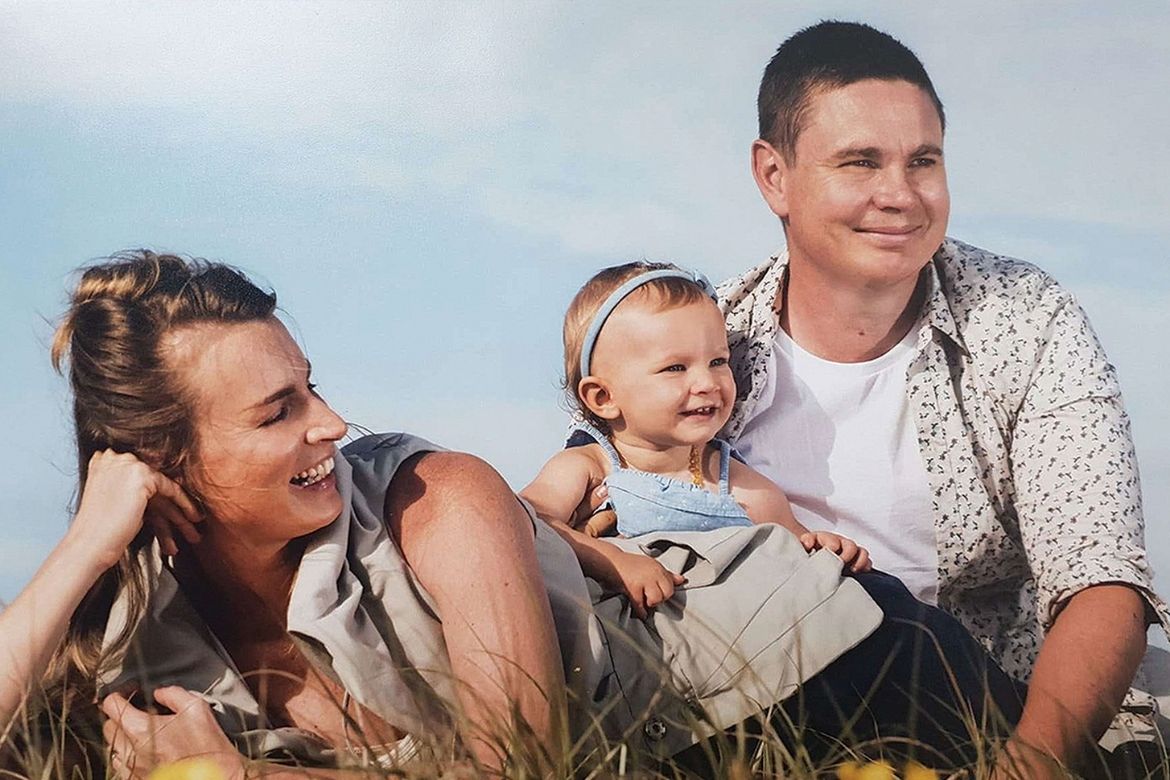
Hi, my name is Peta, I am a mum from Newcastle, N.S.W Australia. I would love to share with you our story: our experiences as first-time parents and how this journey led me to create a unique sleep doll for children.
In late 2016, baby Indie was born with undiagnosed GORD (Gastro-Oesophageal Reflux Disease) and CMPA (Cow’s Milk Protein Allergy), as well as both tongue and lip ties. It wasn’t until day 2 that we knew something was not right. Our baby girl wasn’t latching, and although she looked like she was feeding, she wasn’t properly sucking.
Unfortunately, the pediatrician conducted quick checks on her, buzzing in and out of the hospital room on the morning after she was born. He missed her tongue and lip ties completely, and this was a pivotal moment for us. If he had identified these issues early on, the trouble we all experienced could have been much less, with a simple instant correction.
Indie couldn’t latch to my breast, and she was taking in so much air when trying to feed that it exacerbated her GORD, which she had inherited from both myself and my husband. We were unaware that she had this condition until eight months later when an amazing specialist at the Royal Randwick Hospital diagnosed her.
On day 3, the nurses instructed us to put her on formula because she was losing weight rapidly. As a person who was passionate about natural health, I was initially against this idea. However, my milk came in, and I started developing mastitis because it wasn’t being removed by Indie due to her inability to suck. So, I started pumping my milk heavily with a double breast pump. This helped me overcome the mastitis but only a small amount came out, even though my breasts appeared to be full. The nurses said it wasn’t enough for Indie to exclusively feed.
They kept us in the hospital because they were worried about Indie’s weight. Nurses were all freaking out, arguing all the time and stressed because Indie was so irritable. They all gave conflicting advice, and although lactation consultants tried to help, nothing was working. One midwife waited until the other nurses were out of our room and leaned in close to my face and whispered: “You are better off at home, if I was you I would leave here immediately.”
“The next morning I told them we were going home.”
As first-time parents, we were completely clueless about caring for a newborn, let alone one who was in constant pain. We lost a lot of trust from our hospital experience. For the first few months of Indie’s life, we battled alone while she projectile vomited all day, every day. We hoped it would just ease over time. Eventually seeking help, we visited specialist after specialist, but no one could identify the cause of her symptoms, leaving us feeling helpless and frustrated. Indie cried incessantly, day and night, and the stench of acid permeated our home and clothing, even after deep cleaning.
The nights were especially difficult as she was more irritable, and her first sleep wouldn’t come until 1:30 am every night/morning. Her body would eventually crash from the continuous screaming and back arching, but after a short nap, she would wake up screaming again, and nothing we would do seemed to help. I researched constantly, trying to figure out the root of her pain, and thought maybe Tresillian could help since they specialised in baby sleep. But after spending a week there, they couldn’t offer any solutions since Indie’s issues were health-related. I didn’t know what to do next as I hoped it would all be resolved at Tresillian.
While at Tresillian, I researched cow’s milk protein allergy as Indie exhibited all the symptoms, so I requested a tub of non-cow’s milk formula from a visiting doctor. The first feed of the formula showed a huge reduction in Indie’s crying and arching, but she was still projectile vomiting. I took her to see an immunologist who prescribed the same formula, made from potatoes, which is not ideal for a health-conscious mother like myself as there is basically no nutrition. Nonetheless, it helped her gut, and when I changed my diet to be dairy and soy-free, her symptoms further improved.
Although a lot less, Indie still displayed pain symptoms of screaming and arching, and her skin still emitted a strong acid smell. However I noticed she was less irritated when given my breast milk rather than the formula. One day, she stopped taking the formula entirely. She had her one cup/a small bottle of my breast milk, but when it came to feeding her the formula, she refused it completely each time I offered it, tight lipped and turning her head away with a high pitched scream.
“That day was a bad day that will stay with me forever as the screaming was unforgettable and I was freaking out alone with no idea what to do next.”

I had heard stories of babies rejecting their feeds and having to be tube-fed, and I would have done anything to avoid that. For 18 hours, Indie consumed barely anything. Although I had heard of milk donors before, I never thought it would be necessary for us. However, I had no more milk left to feed her. At that moment, I was running out of ideas, so I quickly sought help to find a local milk donor community. I knew nothing about milk donors, but what I learned fast was that getting a milk donor wasn’t easy, especially a milk donor who wasn’t consuming any dairy or soy and wasn’t on any medications.
One local mother contacted me who had one cup full of milk to give to Indie. It was such a relief. That feed got her through until the following day, and the next day, we found our next closest donor who was a one-hour drive from us with enough milk to last a few days. Some weeks, we lived day-to-day, driving to get enough milk to feed Indie just for that day. However, some donors that were 2-4 hours away were able to produce enough for us to have milk for 2-4 weeks. These big donations were such a relief, as we could breathe for a few weeks without worrying about where the next lot was coming from.
Although Indie was still not sleeping, her symptoms had improved, most notably her stomach not being rock-hard and like a balloon. However, she still continued to projectile vomit. I spent six hours per day/night pumping my milk just to get one small bottle to feed her. Being on the breast pump every few hours meant I had my pumping time to research on my iPad (as I had a good technique of balancing the bottles, making my hands free for the tablet)! I figured out she had tongue and lip ties and sought help from two specialists who were experts in the field. Once they corrected the ties, there was another level of instant improvement as her seal around the bottle was more secure, resulting in less wind.
“Unfortunately her ties were corrected too late and even though she wasn’t sucking in air anymore, the window of her learning the special sucking method for drawing in milk from the breast we were told by her feeding specialist was gone, hence why she still wasn’t able to breastfeed when I persisted with her.”
I was devastated, as breastfeeding would have made life so much easier for us, since my milk would have increased from the latching and we wouldn’t have had to run around getting milk donors. However, on the positive side, her air intake while feeding was reduced. It was clear that Indie’s pain was reduced, but she was still irritable and smelling acidic, which meant that something was still not right. I wasn’t going to give up, as I knew she was still experiencing pain.











