Up to one third of women will experience a problem with their pelvic floor at some point in their lives. Understandably, many women feel hesitant about seeking support for such intimate issues. It’s important to know that pelvic floor dysfunction (PFD) is not a normal side effect of bearing children or getting older. Haley of osteoh answers some of the most common pelvic floor questions below.
What is the pelvic floor and why is it important?
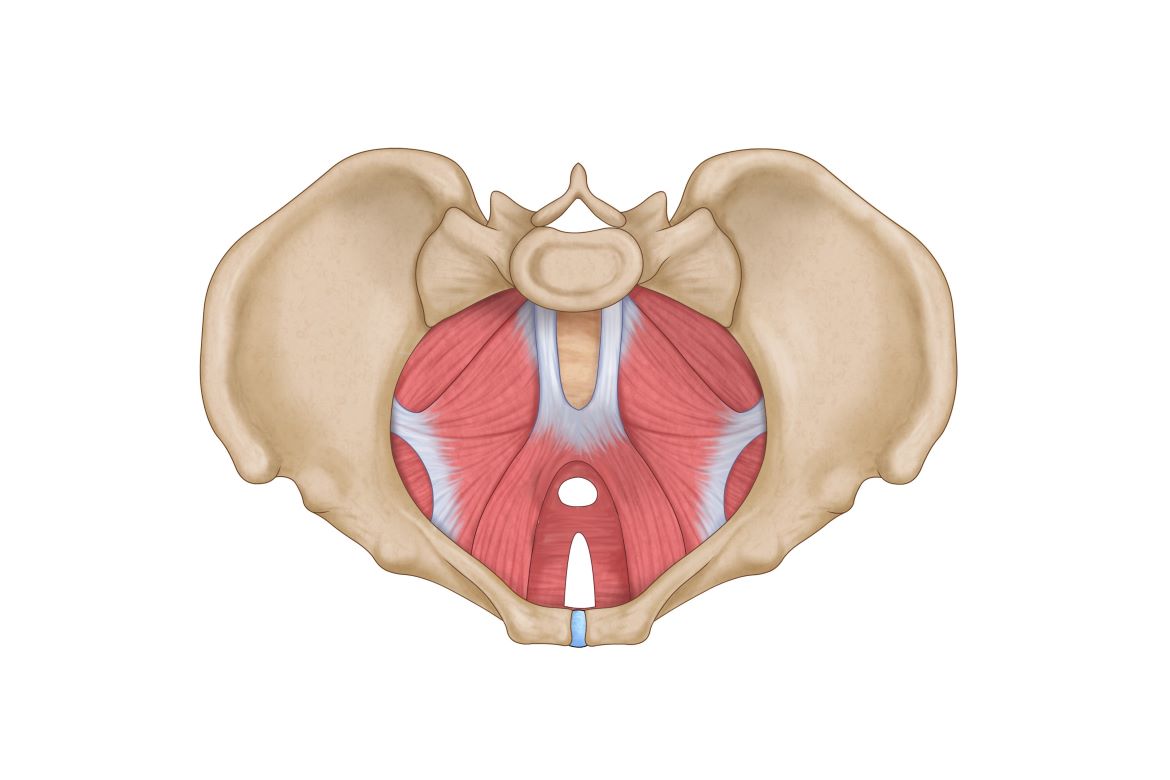
The pelvic floor is a group of muscles and ligaments that provide stability and support to our bladder, bowels and uterus. It provides continence, sexual and birthing function. In pregnancy, the rising up of the uterus squashes our organs, slows bowel function, places excess stress on the spine and abdomen, and increases the pressure on the pelvic floor. Men also have a pelvic floor and can suffer with many of the same issues (minus the vagina and uterus!).
What are the symptoms of an unhappy pelvic floor?
Some common symptoms of PFD are: leaking with cough, sneeze and exercise, wiping three or more times after a poo, pain with intercourse or inserting period products, feelings of heaviness, bulging or dragging in the vagina, difficulty emptying the bladder or bowels, and lower back, hip and tummy pain.
I’m really concerned about prolapse – am I at risk?
Pelvic organ prolapse occurs when there is weakness or damage to the supporting structures of the pelvic floor causing the bladder, rectum or uterus to bulge into the vagina. Women may feel or see tissue protruding from their vagina. However, many women with prolapse have no symptoms at all. The risk of prolapse is greater in women who have vaginal birth, assistance with forceps, chronic constipation and straining, a history of smoking, are obese, menopausal or postmenopausal. Prolapse is treatable with help from a pelvic health therapist. Surgery for prolapse is only required in approximately 10 percent of cases.
Are ‘Kegels’ recommended to fix my pelvic floor dysfunction?
The short answer is ‘it depends’. Unfortunately there is not a one-size-fits-all fix. The recommendations vary for each woman I see depending on their individual activity level, pelvic floor strength and medical history. Many women who are experiencing PFD will clench or tighten their pelvic floor to prevent pain, urgency and leakage. This leads to an ‘overactive’ pelvic floor which means doing kegels will likely worsen their symptoms. An internal assessment of the pelvic floor allows us to determine whether your pelvic floor requires strengthening or stretching and relaxing, and allows us to correctly teach you how to contract, control and relax your pelvic floor muscles properly.
Why is all this important to know?
PFD is more common than you think, but because of the taboo and social embarrassment surrounding this topic, it is widely underreported. Many women I see in clinic have been ‘cleared’ by their midwife or GP, but this rarely means they have had an internal assessment of their pelvic floor. My mission is to normalise the discussion of PFD with family, friends and in the community so that more women can seek treatment early and improve their quality of life and wellbeing. Our bodies go through remarkable changes in a short period of time and we need to honour the recovery.